Substance Use and Mental Health - Unraveling a Complex Web
In the realm of mental health, the interaction between substance use and psychological well-being is a complex and multifaceted. This intricate web of connections can have profound implications for individuals struggling with mental health issues such as depression, anxiety, and social anxiety. In this blog post, we will delve into the scientific understanding of how substance use and mental health intersect, examining the latest research and insights that shed light on this important issue.
To comprehend the interplay between substance use and mental health, it's essential to grasp the foundational concepts. Substance use encompasses a wide range of psychoactive substances, including alcohol, nicotine, prescription medications, and illicit drugs. These substances alter brain chemistry when active in an individual's circulatory and nervous system, leading to various physiological and psychological effects.
The connection between substance use and mental health becomes evident when we consider the impact of these substances on neurotransmitters and brain circuits associated with emotions, stress, and mood regulation. For instance, alcohol and drugs can disrupt the balance of neurotransmitters such as serotonin and dopamine, which play pivotal roles in regulating mood and emotional well-being.
Substance Use and Depression
Depression, a prevalent mental health disorder affecting millions worldwide, is intricately linked with substance use.
Research indicates a bidirectional relationship between the two, where individuals with depression are more prone to substance abuse, and substance use can exacerbate depressive symptoms, and even cause depressive symptoms (with substance misuse of ‘downers’ like barbiturates or benzodiazepines).
The self-medication hypothesis suggests that some individuals turn to substances to alleviate the emotional pain and distress associated with depression. To be fair, it sort of makes sense why this happens - when an individual is suffering, we reach out for something, anything, that may help - and our culture does us no favors when it comes to common cultural ideas around using things like alcohol or cannabis to cope with stress, grief, or to ‘artificially’ change sadness. With that said however, this temporary relief so often leads to a vicious cycle of substance dependence, further worsening their depressive symptoms.
To take this one step further, chronic substance use can directly contribute to the development of depression through alterations in brain chemistry. The prolonged activation of the brain's reward system can result in anhedonia, a common symptom of depression characterized by a diminished ability to experience pleasure.
Ever noticed that it's hard to enjoy things or have much fun when you are hungover? Yep, thats acute anhedonia, not just ‘dehydration and a bad sleep’
Substance Use and Anxiety
Anxiety disorders, including generalized anxiety disorder (GAD) and panic disorder, often co-occur with substance use. Individuals struggling with anxiety may resort to substances as a means of self-medication to reduce their overwhelming feelings of fear and apprehension.
The use of substances like alcohol or benzodiazepines can temporarily alleviate anxiety symptoms. However, the relief is short-lived, and the rebound effect can lead to increased anxiety when the substance's effects wear off. This cycle can perpetuate substance use and exacerbate anxiety disorders.
Have you ever noticed after a night of drinking socially that you are a little more ‘on edge’ the next day? Well that is common and it can increase symptoms of anxiety.
Moreover, chronic substance use can induce physiological changes in the brain, contributing to heightened anxiety levels. This is particularly evident during withdrawal from certain substances, as the body struggles to adapt to the absence of the substance it has become dependent on.
Social Anxiety and Substance Use
Social anxiety, characterized by an intense fear of social situations and interactions, is another mental health condition intertwined with substance use. Of course, most of us are familiar with alcohol - it is the ‘social lubricant’ that helps most people at their office christmas party ease up a bit. Individuals with social anxiety though may turn to substances like alcohol or illicit drugs to ease their social discomfort and boost their confidence in social settings more and more, as it is an ‘easy’ but short-term fix to their anxiety challenge. Of course, there is arguably a ‘healthier’ way to do this, which involves developing a set of coping skills, building up resilience, and building up a tolerance for some.
While substances may provide temporary relief by reducing inhibitions and anxiety, they can also lead to problematic behaviors and substance dependence. Furthermore, long-term substance use can exacerbate social anxiety by eroding an individual's ability to cope with social situations naturally.
The Role of Dual Diagnosis and Integrated Treatment
So, it doesn't really feel good hearing about all the problems - what do I do about this??
Recognizing the intricate relationship between substance use and mental health, mental health professionals have adopted the concept of dual diagnosis or co-occurring issues. Dual diagnosis acknowledges that individuals often face both substance use and mental health challenges simultaneously, necessitating a holistic and integrated treatment approach.
Integrated treatment combines mental health and substance use interventions, aiming to address both aspects comprehensively. This approach recognizes that successful recovery from one condition often requires addressing the other.
We first want to get to your ‘why’:
Why create change?
What problems are you seeing and where do you see them evolving to if you do nothing?
What is the life you want to build for yourself and why?
Next, we will move to really get to understand how mental health challenges cause or interact with a cycle of use or addiction in ones’ life.
How and when do mental health symptoms show up for you?
When do you use your substance? What is the pattern?
Then we create strategies, develop coping skills, and work towards building a healthier and more sustainable life.
Breathing techniques
Self soothing through words, self affirmation, journaling
Exercise
‘Going into the body’ and ‘slowing down’ - meditation, present-ness activities, focusing techniques on ones’ somatic experience
How and when to connect with safe others
Effective and healthy distractions
Lastly, we go move to deeply heal what may be related to, or causing this.
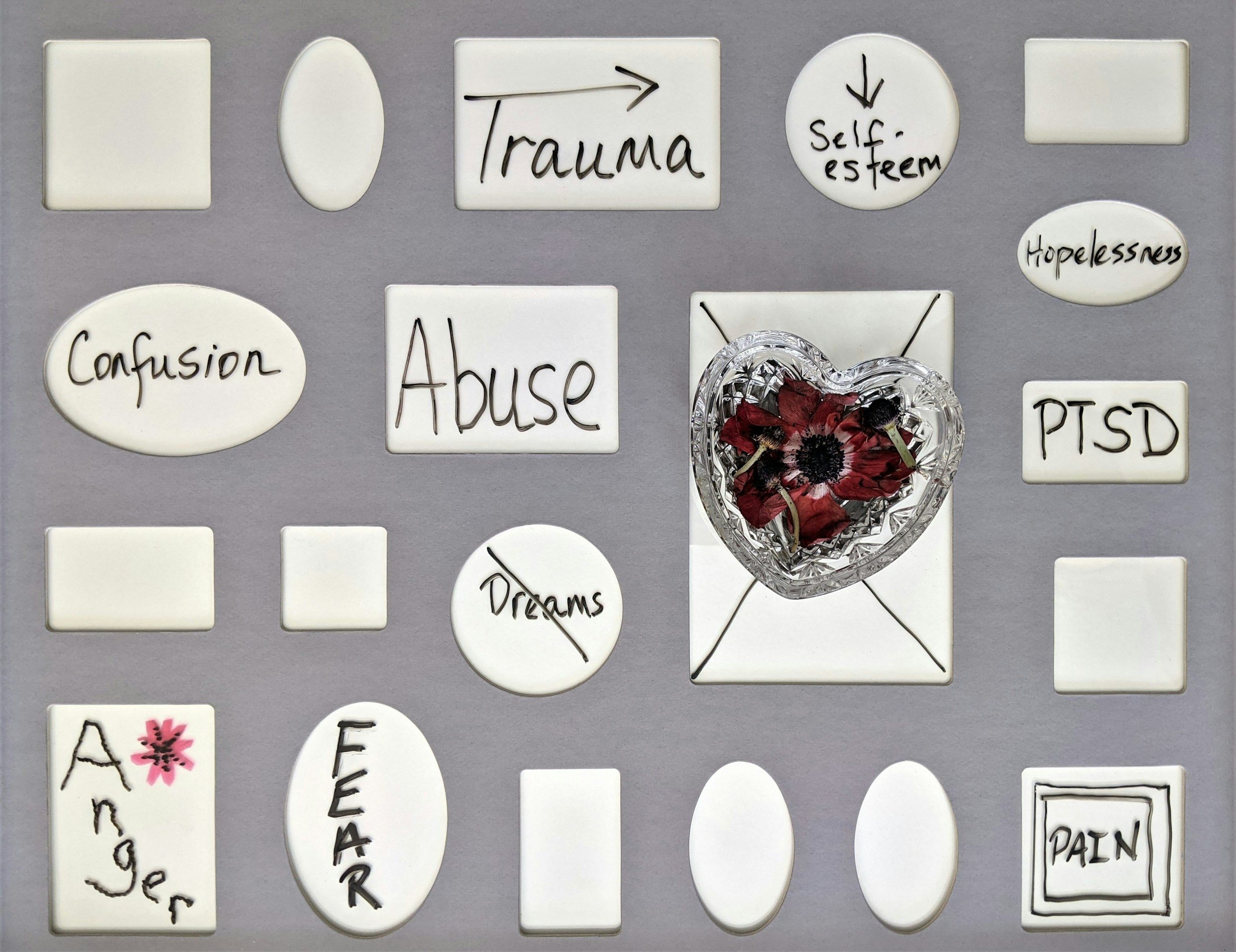
Whether its adverse childhood experiences, pain and shame from enduring years of stigma and ‘what others think’ of ones’ mental health issue, or a trauma
Research has shown that integrated treatment can be highly effective in improving outcomes for individuals dealing with co-occurring disorders, reducing relapse rates, and enhancing overall well-being. Understanding this complex interplay is crucial for mental health practitioners and individuals seeking support. By untangling the threads of substance use and mental health, we can offer more effective interventions, reduce stigma, and ultimately improve the lives of those grappling with these challenges.
In your journey toward mental health and well-being, remember that you are not alone, and there is help available. Reach out to start the process of healing and recovery - we can help.